
Hydrogel Coatings(by J.J.G. Bos) Properties and ApplicationsDesign of Hydrogel Coatings Breakdown Related pages:Note on Staining of HydrogelsAging and Stress Properties and Application of Hydrogels
Hydrogels can be built from various kinds of molecules, thus enabling engineering of a very wide range of functionalities. Think of integration of biodegradable molecules, drugs, lubricious polymers, etc. In addition, the open structure is excellent for post-absorption techniques of e.g. medicine/drugs. This allows for tailoring of the drug-release curves and the starting dose. The hydrogel then serves as what is called an excipient. The lubricious hydrogel coating is one of the most difficult to develop. Reduction of friction is obtained from a combination of molecular mobility - i.e. freedom of movement of hydrophilic functional groups - and the lubricant (water, blood, and so on). Without molecular mobility, hydrogels generally show quite a lot of friction, even when fully hydrated. Just keeping the lubricant in place, hoping for hydroplaning, apparently does not suffice. The greatest problem is to synthesize a hydrogel that maintains sufficient degrees of mobility of the hydrophilic groups, without losing integrity and adhesion. Developers are always bugged by the instability of the low-friction property, because the mobile groups are most often also the ones that do the cross-linking, thus incapacitating each group that reacted. Gradual increase of friction is observed during the cross-linking period, but also after that. This is caused by slow molecular rearrangement (like crystallization), so that the groups as yet lose mobility. Part of it may be recovered after prolonged hydration, so that some hydrogel coatings regain lubricity after prolonged use. Hydrogels must thus be designed with plenty of mobile groups on the one hand, but with sufficient amounts of cross-linking sites on the other. Without that, the gel will easily fall apart. Lack of coating integrity is known to cause particle generation upon clinical use, resulting in an increased risk of complications for the patient. Think of blockage of small coronary and cerebral arteries. Biodegradable hydrogel-based scaffolds are often used for controlled tissue growth. The scaffold itself will eventually fall apart, but it initially acts as growth matrix. This is a method for repairing bone tissue, etc. Unwanted cell-growth sometimes interferes with the intended degradation plan. The undesired growth may follow the shape of the scaffold or even expand on that, thus creating a lump that is there to stay! The result may put pressure on the surrounding nerves and cause permanent pain or even dysfunction of body parts. These are usually long-term effects. Engineering of this type of hydrogel thus requires very extensive biological research. It can be concluded that the versatility of hydrogels is both a blessing and a risk. It is the task for developers to decrease the risk and to emphasize the main functionality. There is no end to the number of materials that are used nowadays to achieve just that, which makes it one of the most difficult but also exciting fields of research.
return to top... Design of Hydrogel Coatings
Coatings made of hydrogels are currently very popular for drug-eluting stents and super-lubricious PTCA balloon-catheters. Other devices, such as relatively floppy super-lubricious catheters for radiology and cardiology have been around for some time now. They are very popular with physicians, because of their ease of operation (especially for distal diagnoses), but the devices are relatively expensive due to coating costs.
 Hydrogel in water. Swelling is limited to 20%. This sample was designed by Cetry for use as intra-ocular lens. When dry, the gel is tough but not hard, when wet it is soft but retains its form, i.e. apart from the limited amount of swelling. return to top... Breakdown of Hydrogel CoatingsHydrogel coatings tend to suffer from the following break-down effects:
Overswelling is generally caused by lack of cross-linking. Early designs of super-lubricious hydrogel coatings lacked sufficient cross-linking and litterally fell apart after some time in the blood. However, overswelling can also be used in a clever way to make sure that the gel works only for a short while and then disintegrates. The latter should not lead to release of gel particles, because that would increase the risk of accute blockage of small blood vessels. Loss of lubricity has been discussed above. Mobility of hydrophilic groups is lost over time due to prolonged cross-linking and molecular setting. More chemical cross-linking leads to less chance of molecular rearrangement, but it also immobilizes more functional groups and access to them. Less cross-linking will leave more mobile groups available, at the risk of overswelling and poor coating adhesion. The long-term effect of loss of lubricity is tough to fight. Investigation is slow, because one cannot use thermally induced accelerated aging in order to study the effect quickly. Real-time monitoring is by far the best method, but who can wait 3 years before deciding whether the coating is good enough? Stress cracking results from forces in the coating layer that become higher than what the bonding-forces can endure in other locations. Coating-thickness is never perfectly homogeneous, so that there are always weak spots to start the cracking. Stress forces increase with coating thickness, cross-linking intensity, and shrinking of the gel. This is why flexible but tough coatings perform much better than hard coatings when it comes to stress cracking. Hydrogel coatings may become detached when the force between the coating and the surface of the medical device is less than the stress force(s) in the bulk of the coating. Mechanical damage can be caused in several ways. Think of bending, scraping and temperature-induced expansion and shrinking. Transportation of hydrogel-coated devices may cause (short) periods of overload of the interfacial forces or the forces inside the coating itself, thus leading to stress cracking and (start of) coating dislodgement. This can be prevented by e.g. making the coating fully compliant with the movement of the substrate or the other way around. Scraping-induced damage generally occurs upon use, i.e. during the clinical procedure. For example: Hydrogel-coated balloon catheters for cardiology are slid through a guiding catheter towards the arterial lesion, thus causing friction between the coating and the guiding catheter. Hydrogel coating particles may be scraped off when the coating is weak (see the note above about overswelling), or when stress-cracking had already damaged the coating too much prior to use. The current generation of super-lubricious coatings generally performs quite well on this subject. Developers evaluate the coating on particle generation under various representative test conditions and make sure that the design eventually complies with the international pharmacopoeias (USP-788-789/EP 2.9.19-20/JP-harmonized with EP and USP) on particulate matter. Biological degradation generally relates to long-term effects in the body. The effects are usually only noted for long-term medical implants. For instance: Hydrogel coatings (on such implants) that use heparin as building block may degrade by cause of heparinase. The blood itself is a very reactive medium and can attack a wide range of molecules (such as heparin). Unwanted biological degradation can often be prevented or slowed down by incorporation of drugs that are designed to positively interact with the reaction balances in the blood. Most difficulties are experienced with so-called inert surfaces/coatings, that in reality cause lots of contact activation by the blood, usually resulting in thrombus formation and inflamation. However, hydrogels tend to dampen these effects quite effectively due to absorption of blood-plasma. This makes the blood in the artery or vein see more body-own material, which in turn leads to no or less response to presence of the coating. E.g. hydrogel coatings on cardiology catheters seem to generate much less thrombus than their uncoated versions. Biological degradation can also be used to clinical advantage. Most biodegradable coatings are designed to degrade under slow reaction with water and eventually leave no trace of their existence. They are designed to perform a temporary job, mostly pacifying the initial negative foreign body response towards medical implants. 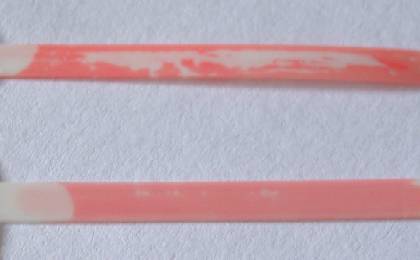 Congo-red induced stress-cracking of a hydrogel. The Congo Red tends to cross-link the hydrogel molecules for this particular recipe. return to top... |